Study unveils Deadly Policy: Hydroxychloroquine Use may have Prevented over 520,000 COVID-19 Deaths in the West

Introduction by Fabio Giuseppe Carlo Carisio
All linked Italian articles ca be read in English thanks to simultaneous machine translation available
The American scientist James Lyons-Weilier has published on his IPAK (Institute for Pure and Applied Knowledge) website a very interesting study (link at the bottom of article) conducted by a university professor of economics from Michigan State University, Mark Skidmore, which analyzed the positive incidence of the use of Hydroxychloriquine against COVID-19 that may have prevented over 520,000 deaths in Western countries where was banned, and at least 420,000 in the US only.
The academic professor discovered that African countries, where it was already routinely used against malaria, noted an enormous benefit compared to those of the European Union and the USA where it was instead excluded from therapies authorized by health bodies after many disputes.
In Italy a legal challenge reached the Council of State, after the Regional Administrative Court of Lazio (TAR in Italian acronymous) had accepted the appeal of an association that opposed the government health protocol of “paracetamol and watchful waiting” highlighting the usefulness of HCQ and Vitamin D.
Despite this, the judges agreed with the Italian Ministry of Health which had opposed the TAR’s decision by continuing to hinder the use of hydroxychloriquine and vitamin D and causing “a record number of deaths in Italy”, as noted by the virologist Maria Rita Gismondo of ‘Sacco Hospital in Milan, to promote the dangerous mRNA vaccines against Covid.
Instead, the French Parliament opened an official inquiry on the on the boycott of HCQ after the Marseille doctor and microbiologist Didier Raoult, specialized in infectious diseases, had highlighted its benefits.
On June, 15, 2020, U.S. Food and Drug Administration (FDA) revoked the emergency use authorization (EUA) that allowed for chloroquine phosphate and hydroxychloroquine sulfate donated to the Strategic National Stockpile to be used to treat certain hospitalized patients with COVID-19 when a clinical trial was unavailable, or participation in a clinical trial was not feasible. The agency determined that the legal criteria for issuing an EUA are no longer met.
Deadly Policy: Peer-Reviewed Cross-Country Study Finds That Routine Hydroxychloroquine Access May Have Prevented Over 520,000 COVID-19 Deaths
by James Lyons-Weilier – originally published on his Substack
All links to previous Gospa News investigations have been added aftermath for the ties with the topics highlighted
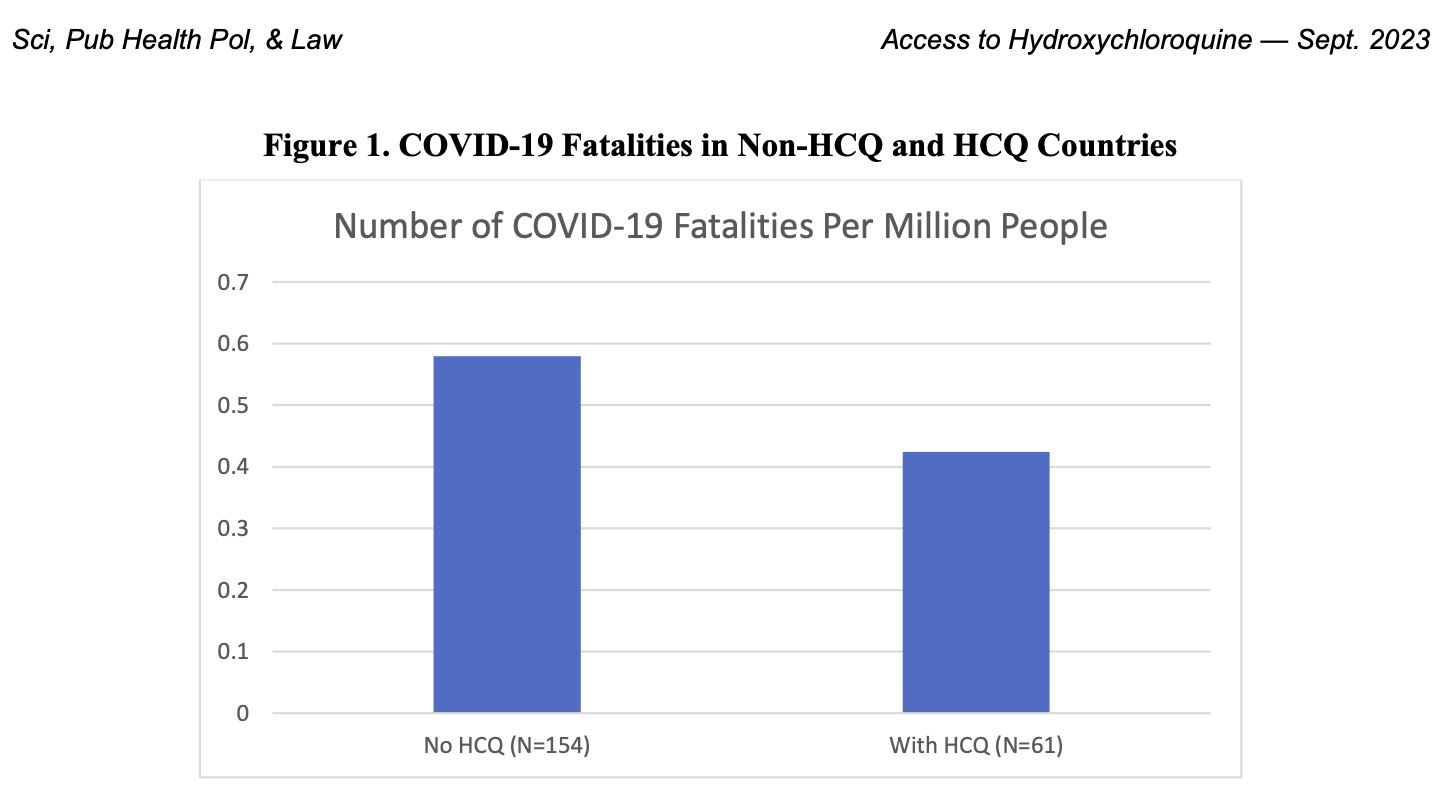
A comprehensive cross-country analysis to identify the factors affecting COVID-19 infections and fatalities found that lack of access to hydroxychloroquine was a major factor in driving COVID-19 deaths.
The study, which was published today in the Public Health Policy Research section of the IPAK PHPI open-access journal, Science, Public Health Policy & the Law (link at the bottom of article), controlled for other variables like obesity, urbanization, age, healthcare infrastructure, and policy responses such as lockdowns and travel restrictions.
A key finding of the studies included was a robust negative relationship between access to HCQ and COVID-19 fatalities. Countries that restricted access to hydroxychloroquine had higher fatalities. The analysis model resulted in an estimate that around 520,000 fatalities could have been avoided if HCQ had been made widely available in countries where it was restricted.
The study also found that obesity, older populations, fewer hospital beds, and less sunshine were associated with higher rates of infection and fatalities.
In contrast to these factors, which were significant across multiple models, national lockdowns were never significantly associated with lowered mortality rates, and local lockdowns were only significantly associated with lowered mortality rates in one model.
The study therefore found that policies like lockdowns, travel restrictions, and mask mandates were generally not associated with a reduction in fatalities. PCR testing was, positively associated with reported infections, but not with fatalities, which the authors attribute to the high false positive rate of the use of non-quantitative PCR testing to assess COVID-19 diagnostic status.
A strong point in the study’s design is the author’s address of the issue of endogeneity. The authors used malaria prevalence as an instrumental variable for HCQ availability and found the result was robust and not due to confounding variables. Endogeneity in this context refers to the potential problem that the relationship between HCQ availability and COVID-19 fatalities might be confounded by unobserved variables or reverse causality. The authors found that endogeneity was not an issue for the relationship between HCQ and fatalities.
Public Health and Policy Implications
The negative association between HCQ availability and fatalities is an important one. Policies on HCQ availability and use should be reconsidered given these results, which should be interpreted in light of the massive compilation of studies that show a net protective effect of early use of hydroxychloroquine in the COVID-19 public health and clinical settings (now 552 studies; c19hcq.org). Countries that have restricted the use of HCQ in the past should now abandon the deadly policy.
HCQ for COVID-19: real-time analysis of all 552 studies (c19hcq.org)
The totality of evidence available on hydroxychloroquine efficacy provides a good starting point for further research and policy discussion.
by James Lyons-Weilier – originally published on his Substack
James Lyons-Weiler (born July 4, 1967) is an American scientist and activist who operates the non-profit organization Institute for Pure and Applied Knowledge (IPAK). He has degrees in zoology, ecology, and conservation biology, and is a former University of Pittsburgh faculty member.
THE RESEARCH
Access to Hydroxychloroquine Is Associated with Reduced COVID-19 Mortality: A Cross-Country Analysis
by Hideki Toya & Mark Skidmore
Dedication: This article is dedicated to my longtime friend, collaborator, and coauthor, Professor Hideki Toya. Professor Toya passed away unexpectedly in 2023. Professor Toya was an insightful and creative researcher. It was a joy to work with him and to count him as a dear friend and colleague.
Correspondence: mskidmor [at] msu.edu, Michigan State University, Agricultural, Food and Resource Economics, East Lansing, MI, USA.
Funding and conflict of interest information: This work was supported by Grant-in-Aid for Research in Nagoya City University Grant Number 2113032. The authors have no conflict of interest.

Abstract
Over the last two and a half years the world experienced the severe acute respiratory syndrome coronavirus 2 (COVID-19) pandemic coupled with unprecedented policy responses. In this article we examine the determinants of COVID-19 infections and fatalities in a cross-country analysis. While our primary objective is to evaluate the role of hydroxychloroquine (HCQ), we also control for other factors that determine vulnerability.
We find that countries that are more obese, less urban, older, have fewer hospital beds, less sunshine, and greater freedom experienced greater fatalities. Generally, policies such as lockdowns, travel restrictions, or mask requirements are unassociated with fatalities. Polymerase chain reaction (PCR) testing is positively associated with reported infections but is unassociated with fatalities.
Controlling for a variety of other determinants of COVID-19 fatalities, we find a robust negative relationship between access to HCQ and fatalities. Estimates indicates that if all countries where HCQ access was restricted had made HCQ available, COVID-19 fatalities would have been reduced by about 520,000.
Some Extracts from Research
Material and methods
COVID-19 infection and fatality data come from the World Health Organization (WHO) [10]. We merge these data with socioeconomic, political, geographic, and policy information from several sources as shown in Appendix Table A. The country is the unit of analysis, where we examine COVID-19 infections per 10 million and fatalities per 100,000 for 128 to 137 countries, depending on data availability.
To evaluate the role of HCQ in reducing infections and fatalities, we control for socio- economic, political, and geographic factors (real gross domestic product [GDP] per capita, obesity, urbanization, proportion of population aged 65 and older, number of hospital beds, degree of freedom, amount of sunshine [11], island country, an indicator variable for whether a country belongs to the Organization for Economic Cooperation and Development [OECD], and policies including PCR testing, travel restrictions, lockdowns, and mask wearing).
We expect countries with lower income, fewer hospital beds, higher urbanicity and proportions of elderly, more freedom, and less sunshine to have more infections and fatalities. Controlling for other policy measures helps to isolate the role HCQ may have in reducing fatalities. These measures are prominent policies that have been used differentially across countries.
HCQ is used in many African countries for the treatment of malaria, and thus the medication is widely available. In contrast, North American and European countries discouraged HCQ use during the COVID-19 pandemic. Appendix Table B provides summary statistics for all variables, and Appendix Table C provides a list of countries included in the evaluation.
Results
The availability of HCQ consistently reduces fatalities in all regressions. According to the coefficient estimate on HCQ in column 2, if the United States had made HCQ widely available, recorded COVID-19 fatalities during the study period would have been reduced from 515,000 to 420,000 [17].
The 2SLS estimation in columns 3 and 5 also have a statistically significant coefficients on HCQ that are roughly twice as large, but the column 2 or 4 estimations are more appropriate given that we find no evidence of endogeneity. Extending the analysis beyond the United States to all countries where HCQ accesswas restricted/unavailable, COVID-19 fatalities would have been reduced by about 520,000 if HCQ had been accessible.
Discussion
This evaluation offers new evidence regarding the potential role that HCQ has played in the COVID- 19 crisis in countries where it was available. However, several caveats are in order. First, the study measures only whether HCQ is available and not whether it was used specifically for COVID-19 in ways the medical literature suggests is most effective.
Second, with cross-country analyses it is possible that confounding factors are not fully accounted for. However, the two-stage least squares analysis reduces this concern to some degree. Third, this type of evaluation should only be considered a supplement to clinical research; clinical research is a more direct approach to examining the efficacy of any medical treatment [19]. Nevertheless, the evaluation offers an important broader perspective on this question.
Research link with Full Text –Science, Public Health Policy & the Law
,
Mark Skidmore
is a tenured Professor and Morris Chair in State and Local Government Finance and Policy, while currently serving as a resident fellow with the MSU Extension Center for Local Government Finance and Policy. He holds tenure system appointments in the Department of Agricultural, Food, and Resource Economics and Economics. He has served as a consultant on a range of issues including economic development, government finance and policy, and price determination. He has published the results of his research in journals such as Economic Inquiry, Economics Letters, Journal of Urban Economics, National Tax Journal, and Public Choice. Much of Skidmore’s research and outreach focuses on public finance policy and the relationship between policy and economic development. Recent research areas include work on property taxation, regional development, and the economics of natural disasters.



